What Is Gender-Affirming Care and Why Do People Need It?
It's a good question, and one I am asked often.
I’m often asked whether gender-affirming care is truly essential, or simply something nice to have. It’s a fair question, especially for people genuinely trying to understand what good, ethical, compassionate healthcare looks like.
What does “gender-affirming care” actually mean?
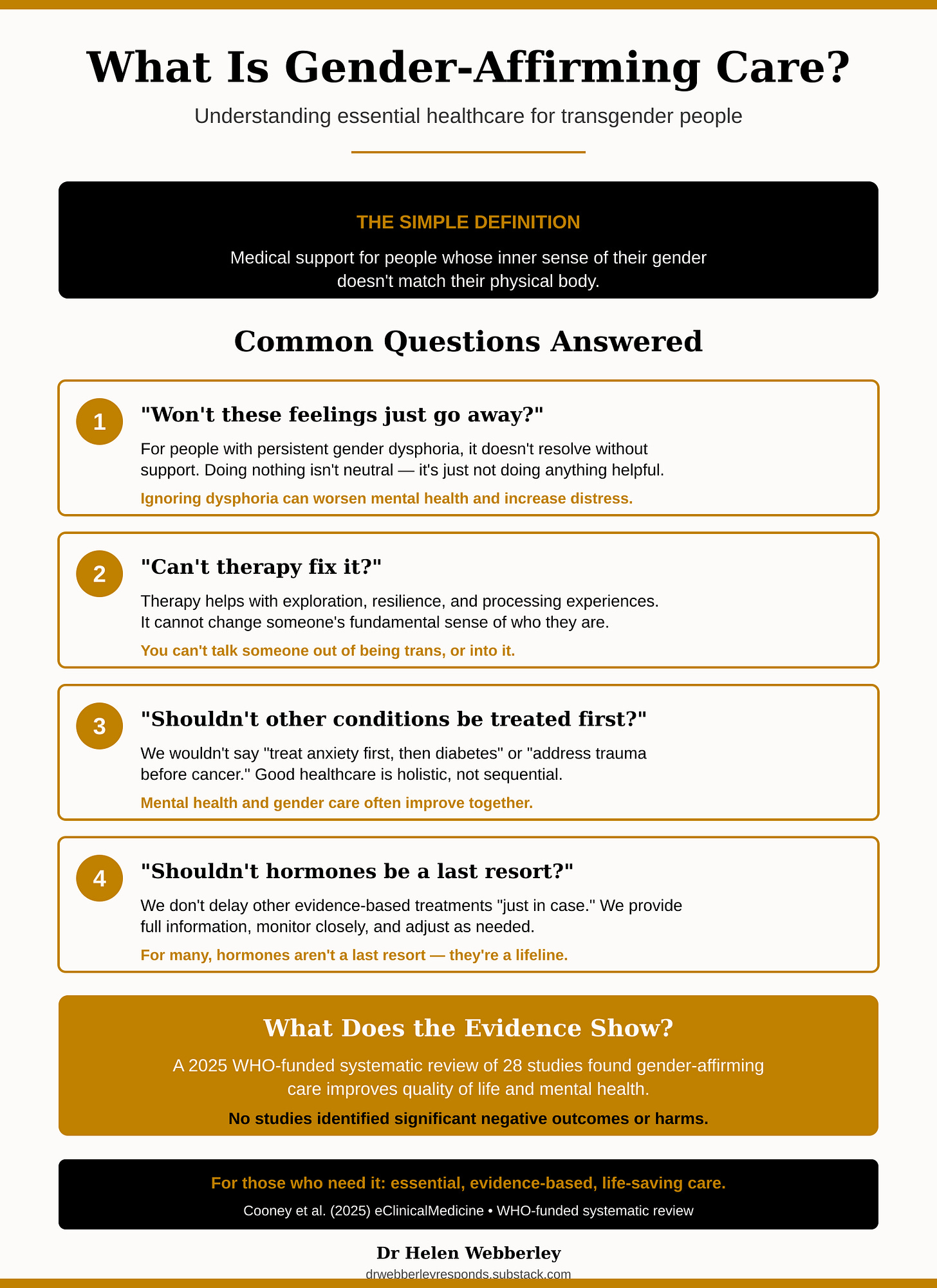
At its simplest, to “affirm” someone means to recognise and respect who they are, without putting up barriers, treating them with suspicion, or making them feel ashamed. For most people, their sense of being male, female, or somewhere in between matches their body, but for some people, there’s a mismatch between how they feel inside and the body they were born with. This mismatch can cause significant distress, known medically as gender dysphoria.
Gender-affirming healthcare is the medical support that helps people whose inner sense of their gender doesn’t match their physical body. This might include counselling, hormone treatments, or sometimes surgery, all provided with careful assessment and ongoing monitoring.
When people ask whether this care is essential or optional, what they usually want to know is: “If we don’t provide hormones or other medical treatments, what happens? Isn’t there something else we could do instead?”
Let me address the most common questions.
“Won’t these feelings just go away on their own?”
Some people do explore questions about their identity and later settle into something different, that’s a normal part of growing up and understanding yourself. However, for people whose gender dysphoria is persistent, deeply felt, and consistent over time, it doesn’t simply resolve without support.
Ignoring the problem, especially in an environment where someone feels rejected or is made to wait indefinitely, can make mental health worse, increase distress, and in too many cases, lead to self-harm or suicide.
Here’s the key point: doing nothing isn’t a neutral choice. It’s still doing something. It’s just not doing anything therapeutic.
“Can’t therapy fix it?”
Talking therapy can absolutely help someone explore their feelings, understand themselves better, build resilience, and process difficult experiences. What it cannot do is change someone’s fundamental sense of who they are.
You can’t talk someone out of being transgender any more than you could talk them into it. Attempts to use therapy as a gatekeeping tool, to “correct” someone’s identity or endlessly delay treatment, have been condemned by every major psychological and medical organisation as both unethical and potentially harmful.
“Shouldn’t other conditions be treated first?”
Many transgender people also experience anxiety, depression, autism, or have a history of trauma, that’s true. But consider how we approach other medical situations.
We wouldn’t say to someone: “Let’s treat your anxiety first, then we’ll deal with your diabetes.” Or: “We need to address your past trauma before we can treat your cancer.”
Good healthcare is holistic. You can support someone’s mental health while also addressing their gender dysphoria. In fact, the two often improve together when appropriate care is provided.
“Shouldn’t hormones be a last resort?”
This is worth questioning. We don’t routinely delay other evidence-based, carefully monitored medical treatments “just in case someone changes their mind.” We work with patients, provide full information so they can give informed consent, monitor closely, and adjust treatment as needed.
For many transgender people, hormone treatment isn’t a desperate final option, it’s the thing that helps them live. Delaying it unnecessarily can make dysphoria worse, allow irreversible physical changes from unwanted puberty to occur, and deepen psychological distress.
So is gender-affirming care essential?
Yes, for the people who need it. This isn’t optional, it’s not cosmetic, it’s not indulgent.
It’s essential, evidence-based and can be life-saving.
This care isn’t given lightly, it’s provided responsibly, ethically, and with careful attention. And when it is provided, the research consistently shows: better mental health, lower suicide risk, and greater life satisfaction.
Medical Reference
Cooney EE et al. (2025). Provision of gender-affirming care for trans and gender-diverse adults: a systematic review of health and quality of life outcomes, values and preferences, and costs. eClinicalMedicine (The Lancet), 79.
This comprehensive WHO-funded systematic review examined 28 studies (including four randomised controlled trials) and found that gender-affirming care may improve quality of life, reduce stigma, increase appropriate use of health services, and improve mental health. Importantly, no studies identified significant negative outcomes or harms.
Full text available at: https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(25)00390-6/fulltext
Dr Helen Webberley | drwebberleyresponds.substack.com